Labour and delivery
Our care team is dedicated to making the birth of your baby the best experience it can be for you and your family.
Before coming to the hospital, it’s important to be prepared for the labour experience. On this page, you will find our recommendations on how you and your family can best prepare for labour and birth.
Hospital Packing List

Essential Items and Documents
Packing list
PRHC Provides
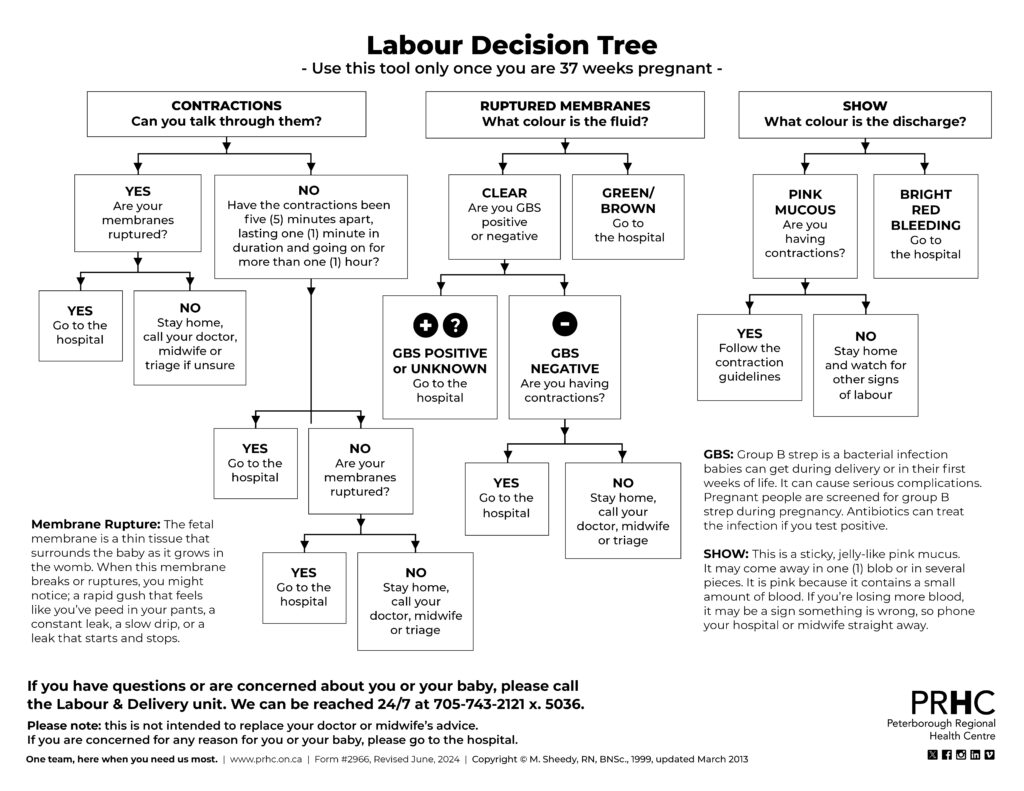
What to do if you are in labour
Your primary care provider, whether an OBGYN, midwife or family physician, may have special instructions about going to the hospital
- At 20 weeks pregnant, or further along, you should come to Labour & Delivery if:
- You’ve been contracting every five (5) minutes, the contractions are lasting at least one (1) minute, and have been happening for at least one (1) hour
- Your contractions are strong enough that you are finding it difficult to talk through them
- You have experienced any gushes of fluid that make you believe your water may have broken
- You are bleeding
- You notice a decrease in your baby’s movements (your baby should move at least six (6) times in two (2) hours)
- Your healthcare provider has advised you to come to the hospital
- Or if you feel the need to come to the hospital for any other reason
- If you are fewer than 20 weeks pregnant, you will be seen in the Emergency Department.
Upon arrival, you will be directed to the assessment room where your nurse or midwife will gather information as to why you’ve come. Please be sure to let them know if you have any special considerations in pregnancy, such as high blood pressure or diabetes.
Pain Management During Labour
During labour you will have a dedicated one-to-one nurse or midwife. Our goal is to ensure that you are comfortable and empowered to use strategies that bests suits you. We will answer any questions you might have along the way.
We have a number of pain management options available for you.
Unmedicated pain management options include:
- Hydrotherapy
- Massage
- Birthing balls and peanut balls
- Distraction and positioning techniques
- Anything else you may need to occupy yourself or to relax you during labour
Medicated pain management options include:
- A combination of nitrous oxide (laughing gas) and oxygen may be self-administered by the patient to provide pain relief during labour and delivery. Nitrous oxide assists in reducing pain but it does not eliminate pain. Nitrous oxide is safe and does not make your baby sleepy. Some women may feel slightly dizzy and disoriented. Nitrous oxide is mostly used in the transitional stage of labour, but can also be used while waiting for an epidural if there is a long wait time.
- Narcotics are sometimes offered in early labour. Nubain is the most common narcotic for this purpose and may be given intramuscularly. Pain relief takes effect within 20 to 30 minutes and lasts from two to four hours. Gravol is usually given together with Nubain to prevent nausea. Sleepiness can be a side-effect for both you and possibly the baby. For this reason, narcotics are usually used in early labour only. The narcotic that is ordered for you is at the discretion of the attending doctor.
- Epidurals are the most effective and widely accepted method of pain relief for labour and birth. A combination of local anesthetic and narcotic is injected into the epidural space to reduce or eliminate pain in the lower body. You will not experience drowsiness as you do with most other methods of pain relief. The epidural allows for ongoing pain relief through labour and birth, and is safe for the baby.
Here at PRHC, we respect your individual choice and will make every effort to accommodate our patients’ birth plans through safe and effective care measures
Preparing for c-section

The day before your surgery: Your care provider may request that you complete your required bloodwork the day before your surgery. If so, you will receive information during one of your antenatal appointments. The bloodwork will be completed by the Outpatient Lab, located on the fifth floor. If you have not completed your bloodwork prior to the day of surgery, please ensure you arrive to Labour and Delivery for 6:45 a.m. on the day of your surgery and let your nurse know so the bloodwork can be completed in a timely manner.
The day of your surgery: We advise that you do not wear contact lenses or jewelry, including body piercings. Please remove all nail polish and inform us if you are unable to remove your piercings.
What can I eat and drink before my surgery? The evening before your surgery you may eat and drink normally. You must stop eating eight hours prior to your caesarean section (midnight). However, you may continue to drink clear fluids up to two (2) hours before the procedure. If you are on medication and are instructed to take it on the day of your surgery, you may take it with a sip of water only.
Where do I go? On the day of your surgery, please arrive to Labour & Delivery by 7:00 a.m. If you did not have bloodwork completed the day prior, we ask that you please arrive by 6:45 a.m. Your care providers will explain procedures as they happen. If you have any questions, please ask.
- Our clerical staff will ask for your Health Card to complete the registration process.
- You will get changed into a hospital gown. Your nurse will take a medical history, listen to your baby’s heart rate, and check your blood pressure, heart rate and temperature.
- An anesthesiologist, the physician who will administer your anesthesia during surgery, will come to speak with you about your medical history, the options for anesthesia (spinal, epidural or general anesthesia) as well as your postoperative pain relief plan.
- An intravenous (IV) line will be started.
- Your nurse will take you to the operating room and help prepare you for your anesthetic.
After your caesarean: You can expect your length of stay in hospital to be approximately 48 hours from time of newborn delivery.
- We encourage you to take your pain medication as directed. Pain relief will help in your recovery by allowing you to get up and move around more easily.
- Getting out of bed and moving around will help you to feel better. We recommend that you sit at the side of your bed and dangle your legs with assistance from your nurse at approximately six hours after your surgery. Please let your nurse help you get out of bed the first time.
- Supporting your incision with a pillow during activity may help reduce your pain.
- Your abdominal dressing will be removed on the second day after your caesarean section, at which time you will be able to have a shower.
- Your surgeon will use either staples or stitches to close your incision. The stitches used to close your incision are dissolvable and will not be removed before you are discharged home. If you have staples, your surgeon will arrange a follow-up appointment for removal. You will be given a prescription for pain relievers to take at home when you need them.
- Gas movement can cause some discomfort. Try these methods to increase your comfort:
- Walk in the hallways
- When lying, change your position from side to side.
- Drink lots of fluids
- Avoid carbonated (fizzy) drinks
What should I do if I go into labour? If you go into labour before your planned caesarean section, go to the Emergency Department to be triaged to labour and delivery. PLEASE DO NOT EAT OR DRINK UNTIL YOU ARE ASSESSED.
If you have any questions, please ask any of your healthcare providers.


